Day to day illness denial means people are missing out on benefits of the huge advances in healthcare which are enabling more to live healthy lives for longer and AIG believes that being realistic and practical about the likelihood of falling ill can help millions benefit from rising longevity across the UK.
The detailed study shows hope is beating reality – just 22 per cent questioned expect to be affected by cancer in their lifetime. Yet for those born after 1960 the risk statistically is 50 per cent, which adds up to 14.2 million living in a state of cancer denial alone.
The reality is that data shows 38 per cent of cancer cases including lung, bowel and skin melanoma are preventable with lifestyle changes. Early diagnosis also has a huge impact on survival chances with NHS cancer screenings, which are in place for bowel, breast and cervical cancer, providing a vital service.
Research shows illness denial affects heart disease too - only 17 per cent believe they will be affected while official statistics show heart and circulatory diseases cause more than a quarter (26 per cent) of all deaths. Strokes are the leading cause of death and disability in the UK but only seven per cent believe it could affect them.
Taking a realistic approach and accepting illness is highly likely to deliver real benefits in not only taking preventative health steps, such as exercise and dietary change, but also in deciding on financial protection which can help with returning to work after illness or providing support if people cannot work.
Over three quarters (77 per cent) of adults say they would experience financial problems if they developed a serious illness in the next six months, with 26 per cent saying they would have significant financial problems.
Having financial protection in place would relieve the potential pressure on family and friends - around a third (34 per cent) of people say they need would rely on friends and family for financial support if they suffered serious illnesses in later life.
There is good news on illness denial – the older we get the more realistic we become. Only around 27 per cent of those aged over 55 years old are convinced serious medical conditions will never happen to them compared with 44 per cent of younger people
Debbie Bolton, Head of Underwriting and Claims Strategy at AIG Life, commented: “Illness denial is understandable as nobody wants to think about the worst happening to them and we all like to believe it won’t be us or our loved ones.
“It’s comforting to know that we are all living longer and Government statistics show that around one in three children born today can expect to live to see their 100th birthday and their parents and grandparents can look forward to long lives too. However, our extended lives mean we may live in poor health for longer and sometimes with more than one serious illness.
“Taking a realistic and practical approach to the risk of illness and the need for financial protection will help us all to plan for the future. If we also take steps to improve our lifestyle we can move into our later years in good health.”
Chartered psychologist and scientist Dr Meg Arroll added: “The AIG Life survey highlights the fundamental disconnect between public health information and individuals’ beliefs of their own risk of illness. In other words, even though there have been numerous campaigns which clearly state the high frequency of health conditions like cancer, heart disease and stroke, this information does not directly equate to individuals’ personal perception of risk.
“Research shows that many people demonstrate an optimism bias, whereby they believe they are less likely to experience key health conditions than data would suggest. Cognitive factors that lead to this misconception include: a lack of personal experience of a condition: a belief that if symptoms have not yet appeared, they are unlikely to in the future; believing that a condition is uncommon.
“In addition, our evaluation of our own illness risk is based on selective focus. For example, many people diminish their own risk-increasing behaviours such as poor diet, smoking and lack of exercise and justify these in terms of the risk-reducing actions they are engaged in (“Even though I don’t exercise regularly, I try to eat my five-a-day so overall I’m healthy”). There is also a proximal aspect in play here – it can be difficult to forego immediate rewards in order to prevent poor health outcomes in the distant future, particularly in situations of low perceived control, self-efficacy and motivation. Therefore, health behaviour change programmes must not only educate us about our risks of developing illness, they should also address cognitive errors such as optimism bias which lead to health-limiting behaviours.”
Regional findings
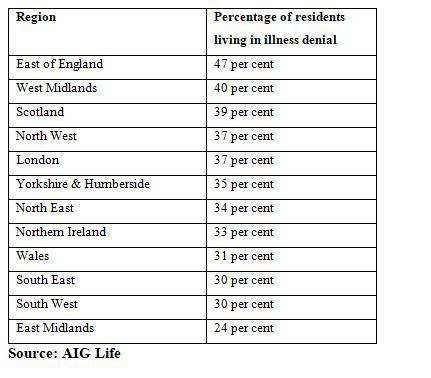
Illness denial is highest in the East of England with almost half (47 per cent) believing they won’t be affected by one of the major causes of death including cancer, stroke and heart disease in their lifetime. People in the East Midlands are the most realistic, with less than a quarter (24 per cent) living in a state of illness denial.
Table one: The regional breakdown of illness denial
|

